«وارفارين»: الفرق بين المراجعتين
(←ضبط الجرعة الفعالة Dosing) |
(←Contraindications) |
||
| سطر 54: | سطر 54: | ||
Patients are making increasing use of self-testing and home monitoring of oral anticoagulation. International guidelines on home testing were published in 2005.<ref name="Ansell2005">{{cite journal |author=Ansell J, Jacobson A, Levy J, Völler H, Hasenkam JM|title=Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation |journal=Int. J. Cardiol. |volume=99 |issue=1|pages=37–45|date=March 2005 |pmid=15721497 |doi=10.1016/j.ijcard.2003.11.008|url =http://patientselftesting.com/uploads/Int_Cardio_Journal_-_Patient_Self_Management.pdf}}</ref> The guidelines stated: "The consensus agrees that patient self-testing and patient self-management are effective methods of monitoring oral anticoagulation therapy, providing outcomes at least as good as, and possibly better than, those achieved with an anticoagulation clinic. All patients must be appropriately selected and trained. Currently available self-testing/self-management devices give INR results that are comparable with those obtained in laboratory testing."<ref name=Ansell2005/> A 2006 [[systematic review]] and [[meta-analysis]] of 14 randomized trials showed home testing led to a reduced incidence of complications (thrombosis and major bleeding) and improved the time in the therapeutic range.<ref>{{cite journal |author=Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P |title=Self-monitoring of oral anticoagulation: a systematic review and meta-analysis|journal=Lancet |volume=367 |issue=9508 |pages=404–11 |date=February 2006|pmid=16458764 |doi=10.1016/S0140-6736(06)68139-7|url =http://www.hadassah.org.il/NR/rdonlyres/7DD940DC-E6B5-43FA-8869-288CAE8FF831/7797/Selfmonitoringoforalanticoagulationasystematicrevi.pdf}}</ref> | Patients are making increasing use of self-testing and home monitoring of oral anticoagulation. International guidelines on home testing were published in 2005.<ref name="Ansell2005">{{cite journal |author=Ansell J, Jacobson A, Levy J, Völler H, Hasenkam JM|title=Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation |journal=Int. J. Cardiol. |volume=99 |issue=1|pages=37–45|date=March 2005 |pmid=15721497 |doi=10.1016/j.ijcard.2003.11.008|url =http://patientselftesting.com/uploads/Int_Cardio_Journal_-_Patient_Self_Management.pdf}}</ref> The guidelines stated: "The consensus agrees that patient self-testing and patient self-management are effective methods of monitoring oral anticoagulation therapy, providing outcomes at least as good as, and possibly better than, those achieved with an anticoagulation clinic. All patients must be appropriately selected and trained. Currently available self-testing/self-management devices give INR results that are comparable with those obtained in laboratory testing."<ref name=Ansell2005/> A 2006 [[systematic review]] and [[meta-analysis]] of 14 randomized trials showed home testing led to a reduced incidence of complications (thrombosis and major bleeding) and improved the time in the therapeutic range.<ref>{{cite journal |author=Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P |title=Self-monitoring of oral anticoagulation: a systematic review and meta-analysis|journal=Lancet |volume=367 |issue=9508 |pages=404–11 |date=February 2006|pmid=16458764 |doi=10.1016/S0140-6736(06)68139-7|url =http://www.hadassah.org.il/NR/rdonlyres/7DD940DC-E6B5-43FA-8869-288CAE8FF831/7797/Selfmonitoringoforalanticoagulationasystematicrevi.pdf}}</ref> | ||
| − | ==Contraindications== | + | ==موانع الإستعمال Contraindications== |
| − | + | *وجود حساسية من أي من مكونات الأقراص. | |
| − | + | *الحمل أو إحتمال حدوث الحمل. | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==Adverse effects== | ==Adverse effects== | ||
مراجعة 00:44، 13 فبراير 2015
الوارفارين' (بالإنجليزية: Warfarin ) ويعرف أيضا بأسماء أخرى (Coumadin, Jantoven, Marevan, Lawarin, and Waran) وهو دواء مضاد تخثر، ظهر لأول مرة عام 1948، تم تسويقه أصلاً كمبيد للقوارض. وبعد بضعة سنوات من تسويقه تبين أنه فعال في اتقاء خثار والانصمام في حالات مرضية عديدة (مثل الوقاية من جلطات الأوعية الدموية سواء شرايين أو أوردة). تم إقرار استخدام الوارفارين كدواء في بداية الخمسينات، ولا يزال أكثر الأدوية المضادة للتخثر/التجلط إستخداماً في العصر الحالي.
محتويات
- 1 آلية العمل
- 2 قضايا وإشكاليات
- 3 الإستخدامات الطبية (الاستطبابات)
- 4 مضادات التجلط الأخرى
- 5 ضبط الجرعة الفعالة Dosing
- 6 موانع الإستعمال Contraindications
- 7 Adverse effects
- 8 Overdose
- 9 Interactions
- 10 Pharmacology
- 11 History
- 12 Use as a pesticide
- 13 إشتقاق الإسم
- 14 اقرأ أيضًا
- 15 مراجع
- 16 وصلات خارجية
آلية العمل
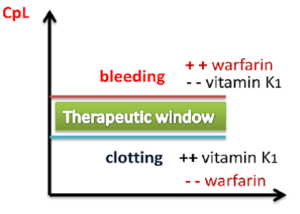
الطريقة التي يعمل بها هذا الدواء تقوم على منع تكوين ڤيتامين K ووهو ڤيتامين ضروري لتصنيع لعدد من عوامل التجلط وهيالعوامل رقم ٢، ٧، ٩، و١٠.وكذلك ضرورى لتصنيع عوامل طبيعية أخرى لمنع التجلط بروتين s وبروتين c لذا، فآن عدم توافر ڤيتامين K يحد من فاعلية عوامل التخثر مما يجعل الدم قليل اللزوجة.
وبالتالي يمكن عكس تأثير الوارفارين عن طريق إعطاء فيتامين ك K لتصنيع عوامل تجلط جديدة ولكن هذا الأثر يأخذ ايام عديدة (من يومان لأسبوع) لظهور هذا الأثر. وباتالي عكس أثر الوارفارين أو أثر زيادة جرعته يأخذ نفس الوقت. يقوم فيتامين ك بتنشيط انزيم الكربوكسيليز ليقوم بإضافة مجموعة كربوكسيل إلى حمض الجلوتاميك في عوامل التجلط وذلك ضروري لعمل رابطة مع طبقة الفوسفولبيد في الأوعية الدموية
قضايا وإشكاليات
إشكالية التداخلات الدوائية
على الرغم من فعالية الوارفارين في منع الجلطات إلا أنه عليه بعض الإشكاليات. مثلاً التداخلات الدوائية والتداخلات الغذائية والحاجة لمتابعة نشاطه بتحليل دوري لسيولة الدم للتأكد من سلامة أداء الدواء وفعالية الجرعة المتناولة.[1]
الإستخدامات الطبية (الاستطبابات)
إستخدام الورفارين غالباً وقائي وليس علاجي. مثلاً في الحالات المرضية التي تتسبب في تكوين خثرات دم بشكل متواصل. من أشهر هذه الحالات الرجفان الأذيني. يستخدم الوارفارين لتقليل القابلية لحدوث جلطات الدم thrombosis أو للوقاية الثانوية (منع تكرار نوبات ثانية) في حالات حدوث الجلطات. الوارفارين بإمكانه منع تكون الجلطات مستقبلاً وتقليل فرصة حدوث السدة الدموية embolism (هجرة جزء من جلطة بالدم إلى مكان أخر في الأوعية الدموية وسد الدورة الدموية)[2].
أفضل نتائجه
أفضل نتائج الوارفارين تحدث عند إستخدامه لمنع الجلطات في الأماكن بطيئة سريان الدم (مثل الأوردة veins والدم المتجمع خلف الصمامات الطبيعية أو الصناعية والدم المتجمع في أذينات القلب المتضخمة. وبالتالي من الأسباب المشهورة لإستعمال الوارفارين حدوث:
- الرجفان الأذيني atrial fibrillation
- صمامات القلب الصناعية artificial heart valves
- جلطة الأوردة العميقة deep venous thrombosis
- السدة الرئوية الدموية pulmonary embolism
كما يستخدم في حالات زيادة تثر الدم المرضية Hypercoagulable state مثل متلازمة مضادات اللبيدات الفوسفورية antiphospholipid syndrome.
كما قد يستخدم أحياناً في منع الجلطات الشريانية مثل جلطات الشريان التاجي ولكن الأهم منه هو إستخدام مضادات الصفائح antiplatelets مثل الأسبرين.[3]
مضادات التجلط الأخرى
توجد بعض الأدوية المضادة للتجلط الأخرى غير الوارفارين.
- أراص بالفم:
- دابيجتران dabigatran (لا يحتاج لمتابعة تحليل سيولة الدم) لكن إستعماله لم يوافق عليه في كل الدول بعد. [4]
- ريفاروكسابان rivaroxaban
ضبط الجرعة الفعالة Dosing
ضبط جرعة الوارفارين عملية معقدة بشدة وتمثل تحدي كبير. وذلك لأن الدواء يتفاعل مع الكثير من الأدوية المستعملة يومياً مع بعض الأغذية.[5] هذه التفاعلات من الممكن أن تقلل أو تزيد فاعلية الوارفارين. These interactions may enhance or reduce warfarin's anticoagulation effect. To optimize the therapeutic effect without risking dangerous side effects such as bleeding, close monitoring of the degree of anticoagulation is required by a blood test measuring an INR. During the initial stage of treatment, INR is checked daily; intervals between tests can be lengthened if the patient manages stable therapeutic INR levels on an unchanged warfarin dose.[3] Newer point-of-care testing is available and has increased the ease of INR testing in the outpatient setting. Instead of a blood draw, the point of care test involves a simple finger prick.[6]
When initiating warfarin therapy ("warfarinization"), the doctor will decide how strong the anticoagulant therapy needs to be. The target INR level varies from case to case depending on the clinical indicators, but tends to be 2–3 in most conditions. In particular, target INR may be 2.5–3.5 (or even 3.0–4.5) in patients with one or more mechanical heart valves.[7]
In addition, for the first three days of "warfarinization", the levels of protein C and protein S (anticoagulation factors) drop faster than procoagulation proteins such as factor II, VII, IX, and X. Therefore, bridging anticoagulant therapies (usually heparin) are often used to reverse this temporary hypercoagulable state.
الجرعة المنتظمة Maintenance dose
Recommendations by many national bodies, including the American College of Chest Physicians,[9] have been distilled to help manage dose adjustments.[10]
The maintenance dose of warfarin can fluctuate significantly depending on the amount of vitamin K1 in the diet. Keeping vitamin K1 intake at a stable level can prevent these fluctuations. Leafy green vegetables tend to contain higher amounts of vitamin K1. Green parts of members of the family Apiaceae, such as parsley, cilantro, and dill, are extremely rich sources of vitamin K; cruciferous vegetables such as cabbage and broccoli, as well as the darker varieties of lettuces and other leafy greens, are also relatively high in vitamin K1. Green vegetables such a peas and green beans do not have such high amounts of vitamin K1 as leafy greens. Certain vegetable oils have high amounts of vitamin K1. Foods low in vitamin K1 include roots, bulbs, tubers, and most fruits and fruit juices. Cereals, grains and other milled products are also low in vitamin K1.[11]
التحليل الذاتي Self-testing
قالب:Main Patients are making increasing use of self-testing and home monitoring of oral anticoagulation. International guidelines on home testing were published in 2005.[12] The guidelines stated: "The consensus agrees that patient self-testing and patient self-management are effective methods of monitoring oral anticoagulation therapy, providing outcomes at least as good as, and possibly better than, those achieved with an anticoagulation clinic. All patients must be appropriately selected and trained. Currently available self-testing/self-management devices give INR results that are comparable with those obtained in laboratory testing."[12] A 2006 systematic review and meta-analysis of 14 randomized trials showed home testing led to a reduced incidence of complications (thrombosis and major bleeding) and improved the time in the therapeutic range.[13]
موانع الإستعمال Contraindications
- وجود حساسية من أي من مكونات الأقراص.
- الحمل أو إحتمال حدوث الحمل.
Adverse effects
Hemorrhage
The only common side effect of warfarin is haemorrhage (bleeding). The risk of severe bleeding is small but definite (a median annual rate of 1 to 3% has been reported[9]) and any benefit needs to outweigh this risk when warfarin is considered as a therapeutic measure. All types of bleeding occur more commonly, but the most catastrophic ones are those involving the brain (intracerebral hemorrhage/hemorrhagic stroke) and the spinal cord.[9] Risk of bleeding is increased if the INR is out of range (due to accidental or deliberate overdose or due to interactions).[14]
A number of risk scores exists to predict bleeding in people using warfarin and similar anticoagulants. A commonly used score (HAS-BLED) includes known predictors of warfarin-related bleeding: uncontrolled high blood pressure (H), abnormal kidney function (A), previous stroke (S), known previous bleeding condition (B), previous labile INR when on anticoagulation (L), elderly as defined by age over 65 (E), and drugs associated with bleeding (e.g. aspirin) or alcohol misuse (D). While their use is recommended in clinical practice guidelines,[15] they are only moderately effective in predicting bleeding risk and don't perform well in predicting hemorrhagic stroke.[16] Bleeding risk may be increased in patients on haemodialysis.[17] Another score used to assess bleeding risk on anticoagulation, specifically Warfarin or Coumadin, is the ATRIA score, which uses a weighted additive scale of clinical findings to determine bleeding risk stratification.[18]
The risks of bleeding are increased further when warfarin is combined with antiplatelet drugs such as clopidogrel, aspirin, or nonsteroidal anti-inflammatory drugs.[19]
Warfarin necrosis
قالب:Main A rare but serious complication resulting from treatment with warfarin is warfarin necrosis, which occurs more frequently shortly after commencing treatment in patients with a deficiency of protein C. Protein C is an innate anticoagulant that, like the procoagulant factors that warfarin inhibits, requires vitamin K-dependent carboxylation for its activity. Since warfarin initially decreases protein C levels faster than the coagulation factors, it can paradoxically increase the blood's tendency to coagulate when treatment is first begun (many patients when starting on warfarin are given heparin in parallel to combat this), leading to massive thrombosis with skin necrosis and gangrene of limbs. Its natural counterpart, purpura fulminans, occurs in children who are homozygous for certain protein C mutations.[20]
Osteoporosis
After initial reports that warfarin could reduce bone mineral density, several studies have demonstrated a link between warfarin use and osteoporosis-related fracture. A 1999 study in 572 women taking warfarin for deep venous thrombosis, risk of vertebral fracture and rib fracture was increased; other fracture types did not occur more commonly.[21] A 2002 study looking at a randomly selected selection of 1523 patients with osteoporotic fracture found no increased exposure to anticoagulants compared to controls, and neither did stratification of the duration of anticoagulation reveal a trend towards fracture.[22]
A 2006 retrospective study of 14,564 Medicare recipients showed that warfarin use for more than one year was linked with a 60% increased risk of osteoporosis-related fracture in men; there was no association in women. The mechanism was thought to be a combination of reduced intake of vitamin K, which is necessary for bone health, and inhibition by warfarin of vitamin K-mediated carboxylation of certain bone proteins, rendering them nonfunctional.[23]
Purple toe syndrome
Another rare complication that may occur early during warfarin treatment (usually within 3 to 8 weeks of commencement) is purple toe syndrome. This condition is thought to result from small deposits of cholesterol breaking loose and causing embolisms in blood vessels in the skin of the feet, which causes a blueish purple colour and may be painful.
It is typically thought to affect the big toe, but it affects other parts of the feet as well, including the bottom of the foot (plantar surface). The occurrence of purple toe syndrome may require discontinuation of warfarin.[24]
Calcification of valves and arteries
Several epidemiological studies have also implicated warfarin use in valvular and vascular calcification. No specific treatment is available, but some modalities are under investigation.[25]
Overdose
The major side effect of warfarin use is bleeding. Risk of bleeding is increased if the INR is out of range (due to accidental or deliberate overdose or due to interactions).[14] Many drug interactions can increase the effect of warfarin, also causing an overdose.[5]
For people who need rapid reversal of warfarin and have serious bleeding or who are having emergency surgery, the effects of warfarin can be reversed with vitamin K with prothrombin complex concentrate or fresh frozen plasma in addition to intravenous vitamin K.[26] Blood products should not be routinely used to reverse warfarin when vitamin K could work alone.[26]
Details on reversing warfarin are provided in clinical practice guidelines from the American College of Chest Physicians.[1] For patients with an international normalized ratio (INR) between 4.5 and 10.0, a small dose (about 1000 mcg = one milligram) of oral vitamin K is sufficient. When warfarin is being given and INR is in therapeutic range, simple discontinuation of the drug for five days is usually enough to reverse the effect and cause INR to drop below 1.5.[27]
Interactions
Warfarin interacts with many commonly used drugs, and the metabolism of warfarin varies greatly between patients.[5] Some foods have also been reported to interact with warfarin.[5] Apart from the metabolic interactions, highly protein bound drugs can displace warfarin from serum albumin and cause an increase in the INR.[28] This makes finding the correct dosage difficult, and accentuates the need of monitoring; when initiating a medication that is known to interact with warfarin (e.g. simvastatin), INR checks are increased or dosages adjusted until a new ideal dosage is found.
Many commonly used antibiotics, such as metronidazole or the macrolides, will greatly increase the effect of warfarin by reducing the metabolism of warfarin in the body. Other broad-spectrum antibiotics can reduce the amount of the normal bacterial flora in the bowel, which make significant quantities of vitamin K1, thus potentiating the effect of warfarin.[29] In addition, food that contains large quantities of vitamin K1 will reduce the warfarin effect.[5][9] Thyroid activity also appears to influence warfarin dosing requirements;[30] hypothyroidism (decreased thyroid function) makes people less responsive to warfarin treatment,[31] while hyperthyroidism (overactive thyroid) boosts the anticoagulant effect.[32] Several mechanisms have been proposed for this effect, including changes in the rate of breakdown of clotting factors and changes in the metabolism of warfarin.[30][33]
Excessive use of alcohol is also known to affect the metabolism of warfarin and can elevate the INR and thus increase the risk of bleeding.[34] The U.S. Food and Drug Administration (FDA) product insert on warfarin states that alcohol should be avoided.[35]
Warfarin also interacts with many herbs and spices,[36] some used in food (such as ginger and garlic) and others used purely for medicinal purposes (such as ginseng and Ginkgo biloba). All may increase bleeding and bruising in people taking warfarin; similar effects have been reported with borage (starflower) oil or fish oils.[37] St. John's Wort, sometimes recommended to help with mild to moderate depression, reduces the effectiveness of a given dose of warfarin; it induces the enzymes that break down warfarin in the body, causing a reduced anticoagulant effect.[38]
Between 2003 and 2004, the UK Committee on Safety of Medicines received several reports of increased INR and risk of haemorrhage in people taking warfarin and cranberry juice.[39][40][41] Data establishing a causal relationship is still lacking, and a 2006 review found no cases of this interaction reported to the FDA;[41] nevertheless, several authors have recommended that both doctors and patients be made aware of its possibility.[42] The mechanism behind the interaction is still unclear.[41]
Pharmacology
Pharmacokinetics
Warfarin consists of a racemic mixture of two active enantiomers—R- and S- forms—each of which is cleared by different pathways. S-warfarin is 2-5 times more potent than the R-isomer in producing an anticoagulant response.[3]
Warfarin is slower-acting than the common anticoagulant heparin, though it has a number of advantages. Heparin must be given by injection, whereas warfarin is available orally. Warfarin has a long half-life and need only be given once a day. Heparin can also cause a prothrombotic condition, heparin-induced thrombocytopenia (an antibody-mediated decrease in platelet levels), which increases the risk for thrombosis. It takes several days for warfarin to reach the therapeutic effect since the circulating coagulation factors are not affected by the drug (thrombin has a half-life time of days). Warfarin's long half-life means that it remains effective for several days after it was stopped. Furthermore, if given initially without additional anticoagulant cover, it can increase thrombosis risk (see below). For these main reasons, hospitalised patients are usually given heparin with warfarin initially, the heparin covering the 3–5 day lag period and being withdrawn after a few days.
Mechanism of action
While warfarin is one of several drugs popularly referred to as a "blood thinner;" this is a misnomer since it does not affect the viscosity of blood.
Warfarin inhibits the vitamin K-dependent synthesis of biologically active forms of the calcium-dependent clotting factors II, VII, IX and X, as well as the regulatory factors protein C, protein S, and protein Z.[1][43] Other proteins not involved in blood clotting, such as osteocalcin, or matrix Gla protein, may also be affected.
The precursors of these factors require carboxylation of their glutamic acid residues to allow the coagulation factors to bind to phospholipid surfaces inside blood vessels, on the vascular endothelium. The enzyme that carries out the carboxylation of glutamic acid is gamma-glutamyl carboxylase. The carboxylation reaction will proceed only if the carboxylase enzyme is able to convert a reduced form of vitamin K (vitamin K hydroquinone) to vitamin K epoxide at the same time. The vitamin K epoxide is in turn recycled back to vitamin K and vitamin K hydroquinone by another enzyme, the vitamin K epoxide reductase (VKOR). Warfarin inhibits epoxide reductase[44] (specifically the VKORC1 subunit[45][46]), thereby diminishing available vitamin K and vitamin K hydroquinone in the tissues, which inhibits the carboxylation activity of the glutamyl carboxylase. When this occurs, the coagulation factors are no longer carboxylated at certain glutamic acid residues, and are incapable of binding to the endothelial surface of blood vessels, and are thus biologically inactive. As the body's stores of previously produced active factors degrade (over several days) and are replaced by inactive factors, the anticoagulation effect becomes apparent. The coagulation factors are produced, but have decreased functionality due to undercarboxylation; they are collectively referred to as PIVKAs (proteins induced [by] vitamin K absence/antagonism), and individual coagulation factors as PIVKA-number (e.g.PIVKA-II). The end result of warfarin use, therefore, is to diminish blood clotting in the patient.
When warfarin is newly started, it may promote clot formation temporarily. This is because the level of protein C and protein S are also dependent on vitamin K activity. Warfarin causes decline in protein C levels in first 36 hours. In addition, reduced levels of protein S lead to a reduction in activity of protein C (for which it is the co-factor) and therefore reduced degradation of factor Va and factor VIIIa. Although loading doses of warfarin over 5 mg also produce a precipitous decline in factor VII, resulting in an initial prolongation of the INR, full antithrombotic effect does not take place until significant reduction in factor II occurs days later. The haemostasis system becomes temporarily biased towards thrombus formation, leading to a prothrombotic state. Thus, when warfarin is loaded rapidly at greater than 5 mg per day, it is beneficial to co-administer heparin, an anticoagulant that acts upon antithrombin and helps reduce the risk of thrombosis, with warfarin therapy for four to five days, in order to have the benefit of anticoagulation from heparin until the full effect of warfarin has been achieved.[47][48]
Pharmacogenomics
Warfarin activity is determined partially by genetic factors. Polymorphisms in two genes (VKORC1 and CYP2C9) play a particularly large role in response to warfarin.
VKORC1 polymorphisms explain 30% of the dose variation between patients:[49] particular mutations make VKORC1 less susceptible to suppression by warfarin.[46] There are two main haplotypes that explain 25% of variation: low-dose haplotype group (A) and a high-dose haplotype group (B).[50] VKORC1 polymorphisms explain why African Americans are on average relatively resistant to warfarin (higher proportion of group B haplotypes), while Asian Americans are generally more sensitive (higher proportion of group A haplotypes).[50] Group A VKORC1 polymorphisms lead to a more rapid achievement of a therapeutic INR, but also a shorter time to reach an INR over 4, which is associated with bleeding.[51]
CYP2C9 polymorphisms explain 10% of the dose variation between patients,[49] mainly among Caucasian patients as these variants are rare in African American and most Asian populations.[52] These CYP2C9 polymorphisms do not influence time to effective INR as opposed toVKORC1, but does shorten the time to INR >4.[51]
Despite the promise of pharmacogenomic testing in warfarin dosing, its use in clinical practice is controversial. In August 2009 the Centers for Medicare and Medicaid Services concluded that "the available evidence does not demonstrate that pharmacogenomic testing of CYP2C9 or VKORC1 alleles to predict warfarin responsiveness improves health outcomes in Medicare beneficiaries."[53] A 2014 meta-analysis showed that using genotype-based dosing did not confer benefit in terms of time within therapeutic range, excessive anticoagulation (as defined by INR greater than 4), or a reduction in either major bleeding or thromboembolic events.[54]
History
In the early 1920s, there was an outbreak of a previously unrecognised cattle disease in the northern United States and Canada. Cattle were haemorrhaging after minor procedures, and on some occasions, spontaneously. For example, 21 out of 22 cows died after dehorning, and 12 out of 25 bulls died after castration. All of these animals had bled to death.[55]
In 1921, Frank Schofield, a Canadian veterinary pathologist, determined that the cattle were ingesting moldy silage made from sweet clover that functioned as a potent anticoagulant. Only spoiled hay made from sweet clover (grown in northern states of the USA and in Canada since the turn of the century) produced the disease.[56] Schofield separated good clover stalks and damaged clover stalks from the same hay mow, and fed each to a different rabbit. The rabbit that had ingested the good stalks remained well, but the rabbit that had ingested the damaged stalks died from a haemorrhagic illness. A duplicate experiment with a different sample of clover hay produced the same result.[55] In 1929, North Dakota veterinarian Dr L.M. Roderick demonstrated that the condition was due to a lack of functioning prothrombin.[57]
The identity of the anticoagulant substance in spoiled sweet clover remained a mystery until 1940. In 1933 Karl Paul Link and his lab of chemists working at the University of Wisconsin set out to isolate and characterize the haemorrhagic agent from the spoiled hay. It took five years for Link's student Harold A. Campbell to recover 6 mg of crystalline anticoagulant. Next, Link's student Mark A. Stahmann took over the project and initiated a large-scale extraction, isolating 1.8 g of recrystallized anticoagulant in about 4 months. This was enough material for Stahmann and Charles F. Huebner to check their results against Campbell's and to thoroughly characterize the compound. Through degradation experiments they established that the anticoagulant was 3,3'-methylenebis-(4-hydroxycoumarin), which they later named dicoumarol. They confirmed their results by synthesizing dicoumarol and proving in 1940 that it was identical to the naturally occurring agent.[58]
Dicoumarol was a product of the plant molecule coumarin (not to be confused with Coumadin, a later tradename for warfarin). Coumarin is now known to be present in many plants, and produces the notably sweet smell of freshly cut grass or hay and plants like sweet grass; in fact, the plant's high content of coumarin is responsible for the original common name of "sweet clover", which is named for its sweet smell, not its bitter taste.[55] They are present notably in woodruff (Galium odoratum, Rubiaceae), and at lower levels in licorice, lavender, and various other species. However, coumarins themselves do not influence clotting or warfarin-like action, but must first be metabolized by various fungi into compounds such as 4-hydroxycoumarin, then further (in the presence of naturally occurring formaldehyde) into dicoumarol, in order to have any anticoagulant properties. Fungal attack of the damaged and dying clover stalks explained the presence of the anticoagulant only in spoiled clover silages; dicoumarol is considered to be a fermentation product and mycotoxin.[59]
Over the next few years, numerous similar chemicals (specifically 4-hydroxycoumarins with a large aromatic substitutent at the 3 position) were found to have the same anticoagulant properties. The first drug in the class to be widely commercialized was dicoumarol itself, patented in 1941 and later used as a pharmaceutical. Karl Link continued working on developing more potent coumarin-based anticoagulants for use as rodent poisons, resulting in warfarin in 1948. The name "warfarin" stems from the acronym WARF, for Wisconsin Alumni Research Foundation + the ending -arin indicating its link with coumarin. Warfarin was first registered for use as a rodenticide in the US in 1948, and was immediately popular. Although warfarin was developed by Link, the Wisconsin Alumni Research Foundation financially supported the research and was assigned the patent.[60]
After an incident in 1951, where a US Army inductee unsuccessfully attempted suicide with multiple doses of warfarin in rodenticide and recovered fully after presenting to a hospital, and being treated with vitamin K (by then known as a specific antidote),[60] studies began in the use of warfarin as a therapeutic anticoagulant. It was found to be generally superior to dicoumarol, and in 1954 was approved for medical use in humans. An early recipient of warfarin was US president Dwight Eisenhower, who was prescribed the drug after having a heart attack in 1955.[60]
The exact mechanism of action remained unknown until it was demonstrated, in 1978, that warfarin inhibits the enzyme epoxide reductase and hence interferes with vitamin K metabolism.[44]
It has been theorized that Lavrenty Beria, Nikita Khrushchev and others conspired to use warfarin to poison the Soviet leader Joseph Stalin. Warfarin is tasteless and colourless, and produces symptoms similar to those that Stalin exhibited.[61]
Use as a pesticide

To this day, the so-called "coumarins" (4-hydroxycoumarin derivatives) are used as rodenticides for controlling rats and mice in residential, industrial, and agricultural areas. Warfarin is both odorless and tasteless, and is effective when mixed with food bait, because the rodents will return to the bait and continue to feed over a period of days until a lethal dose is accumulated (considered to be 1 mg/kg/day over about six days). It may also be mixed with talc and used as a tracking powder, which accumulates on the animal's skin and fur, and is subsequently consumed during grooming. The قالب:LD50 is 50–500 mg/kg. The IDLH value is 100 mg/m3 (warfarin; various species).[62]
The use of warfarin itself as a rat poison is now declining, because many rat populations have developed resistance to it, and poisons of considerably greater potency are now available. Other 4-hydroxycoumarins used as rodenticides include coumatetralyl and brodifacoum, which is sometimes referred to as "super-warfarin", because it is more potent, longer-acting, and effective even in rat and mouse populations that are resistant to warfarin. Unlike warfarin, which is readily excreted, newer anticoagulant poisons also accumulate in the liver and kidneys after ingestion.[63]
إشتقاق الإسم
تم إكتشاف الوارفارين في البرسيم الحلو المعطب spoiled sweet clover أثناء إستخدامه كغذاء حيواني. لفظ وارفارين Warfarin تم إشتقاقه من مختصر الحروف الأولى Acronym للمشروع العلمي الذي إكتشفه. وهو مشروع "وارف" "WARF" مؤسسة أبحاث خريجيي وسكينسن Wisconsin Alumni Research Foundation ثم تم إضافة النهاية "ارين" له"-arin" للدلالة على إنتماءه للمجمعة الأدوية كومارين Coumarin.
حاسبات فرصة حدوث النزيف Online Bleeding Risk Calculators
- ATRIA Bleeding Risk Score from MDCalc
- HAS-BLED Score from MDCalc
اقرأ أيضًا
مراجع
- https://ar.wikipedia.org/wiki/%D9%88%D8%A7%D8%B1%D9%81%D8%A7%D8%B1%D9%8A%D9%86
- https://en.wikipedia.org/wiki/Warfarin
وصلات خارجية
- Historical information on warfarin from the Wisconsin Alumni Research Foundation
- Online sweet clover disease and warfarin historical review
- U.S. National Library of Medicine: Drug Information Portal–Warfarin
- Warfarin bound to proteins in the PDB: R-warfarin,S-warfarin
- CDC - NIOSH Pocket Guide to Chemical Hazards
- Pesticide Properties DataBase (PPDB)
- {{#if:طب | قالب:شريط بوابة طب |
- خطأ في استعمال قالب:شريط بوابات: يلزم إعطاء وسيط واحد على الأقل. }}{{#if:صيدلة | قالب:شريط بوابة صيدلة }}{{#if: | {{شريط بوابة {{{3}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{4}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{5}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{6}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{7}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{8}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{9}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{10}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{11}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{12}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{13}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{14}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{15}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{16}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{17}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{18}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{19}}}|أصلية=شريط}} }}{{#if: | {{شريط بوابة {{{20}}}|أصلية=شريط}} }}{{#if: |
- خطأ في استعمال قالب:شريط بوابات: يلزم إعطاء عشرين وسيطا على الأكثر. }}
- ^ 1٫0 1٫1 1٫2 قالب:Cite journal
- ↑ قالب:Cite web
- ^ 3٫0 3٫1 3٫2 قالب:Cite journal
- ↑ قالب:Cite journal
- ^ 5٫0 5٫1 5٫2 5٫3 5٫4 قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite web
- ^ 9٫0 9٫1 9٫2 9٫3 قالب:Cite journal
- ↑ قالب:Cite web
- ↑ قالب:Cite web
- ^ 12٫0 12٫1 قالب:Cite journal
- ↑ قالب:Cite journal
- ^ 14٫0 14٫1 قالب:Cite journal خطأ استشهاد: وسم
<ref>غير صالح؛ الاسم "Garcia2010" معرف أكثر من مرة بمحتويات مختلفة. - ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ^ 26٫0 26٫1 {{ #if: |قالب:Citation/patent |{{#invoke:citation/CS1|citation |CitationClass=citation |separator=، |ref=harv |postscript= }} }}{{#if:|}}
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ^ 30٫0 30٫1 قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ خطأ استشهاد: وسم
<ref>غير صحيح؛ لا نص تم توفيره للمراجع المسماةTGA - ↑ قالب:Cite book
- ↑ قالب:Cite web قالب:Dead link
- ↑ قالب:Cite web
- ↑ قالب:Cite web
- ↑ قالب:Cite journal
- ^ 41٫0 41٫1 41٫2 قالب:Cite journalFree full text with registration at Medscape
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ^ 44٫0 44٫1 قالب:Cite journal
- ↑ قالب:Cite journal
- ^ 46٫0 46٫1 قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ^ 49٫0 49٫1 قالب:Cite journal
- ^ 50٫0 50٫1 قالب:Cite journal
- ^ 51٫0 51٫1 قالب:Cite journal
- ↑ قالب:Cite journal
- ↑ قالب:Cite web
- ↑ قالب:Cite journal
- ^ 55٫0 55٫1 55٫2 قالب:Cite book
- ↑ قالب:Cite journal
- ↑ قالب:Cite journalPDF (subscriber only).
- ↑ قالب:Cite journal
- ↑ قالب:Cite journal
- ^ 60٫0 60٫1 60٫2 قالب:Cite journal
- ↑ قالب:Cite book
- ↑ قالب:Cite web
- ↑ قالب:Cite book